**Narrative Article on Coccyx Physiotherapy Treatment: A Comprehensive Guide**
In the world of physiotherapy, there's a crucial area that often goes unnoticed but can cause significant discomfort and hinder daily activities if not properly addressed: the coccyx, commonly known as the tailbone. At our specialized clinic, we understand the importance of coccyx health and the impact it has on overall well-being. In this comprehensive guide, we'll delve into the intricacies of coccyx issues and how effective physiotherapy treatment can alleviate pain, improve mobility, and enhance your quality of life.
## Understanding the Coccyx
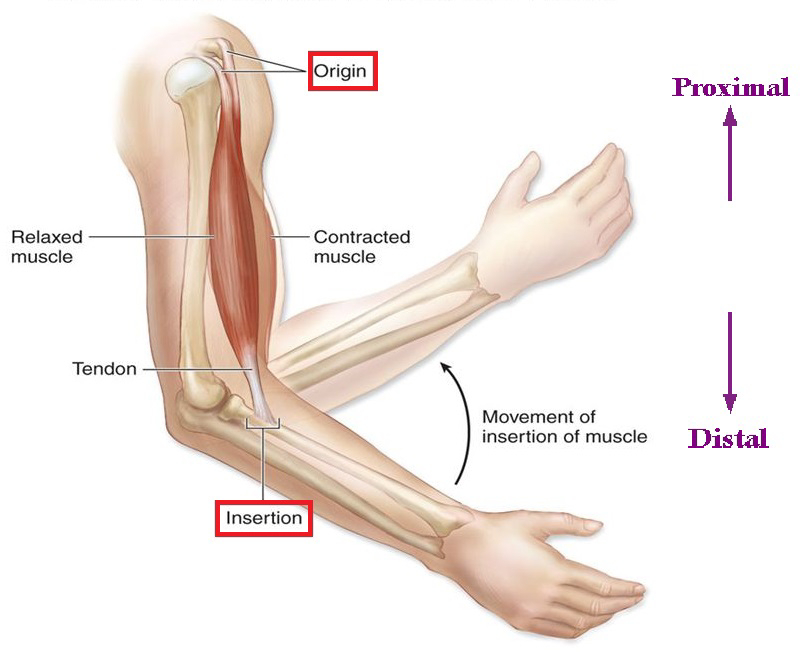
The coccyx is a small triangular bone located at the base of the spine. It consists of three to five fused vertebrae and plays a crucial role in supporting the body while sitting and providing attachment points for various muscles, tendons, and ligaments. Due to its location and function, the coccyx is susceptible to injuries, inflammation, and chronic pain.
## **Common Coccyx Issues**
Several factors can contribute to coccyx-related problems, including trauma from falls, prolonged sitting on hard surfaces, childbirth, or even chronic conditions such as coccydynia (persistent coccyx pain). Individuals experiencing coccyx pain often find it challenging to sit, stand, or engage in physical activities, severely impacting their daily routines and overall comfort.
## **The Role of Physiotherapy**
Physiotherapy is a non-invasive, holistic approach that can significantly alleviate coccyx pain and address related issues. Our experienced physiotherapists employ a personalized approach to assess each patient's condition, create tailored treatment plans, and monitor progress throughout the recovery journey.
### **1. Assessment and Diagnosis**
Our first step is a comprehensive assessment to understand the root cause of the coccyx issue. We consider factors such as medical history, lifestyle, previous injuries, and the specific nature of the pain. This thorough evaluation allows us to pinpoint the underlying problem accurately.
### **2. Tailored Treatment Plans**
Once we've identified the cause of the discomfort, we design a customized treatment plan that may include a combination of manual therapies, gentle exercises, postural adjustments, and ergonomic advice. Our focus is not just on relieving immediate pain but on addressing the root issue to prevent future occurrences.
### **3. Gentle Exercises and Rehabilitation**
Engaging in appropriate exercises is vital for the recovery process. Our physiotherapists guide patients through gentle exercises that strengthen the surrounding muscles, improve flexibility, and enhance overall spinal health. These exercises are crucial for the long-term well-being of the coccyx and the entire spine.
### **4. Pain Management Techniques**
We understand that managing pain is a significant concern for our patients. Our team employs various pain relief techniques, including heat and cold therapy, gentle massage, and relaxation techniques, to alleviate discomfort and promote healing.
### **5. Lifestyle Modifications**
In addition to the direct treatment of the coccyx, we provide valuable guidance on making necessary lifestyle modifications. This includes recommendations for proper sitting posture, using supportive cushions, and incorporating regular movement breaks, especially if you have a sedentary job.
## **Your Journey to Coccyx Wellness**
At our clinic, we're committed to empowering our patients with the knowledge and tools they need to regain coccyx health and overall well-being. Our approach goes beyond short-term relief; we aim for long-lasting results that enable you to live your life to the fullest, free from the constraints of coccyx pain.
If you're ready to embark on a journey towards coccyx wellness and enjoy a life free from discomfort, don't hesitate to reach out to our dedicated team of physiotherapists. We're here to support you every step of the way, helping you regain mobility, comfort, and confidence.
## **Conclusion**
In this comprehensive guide, we've explored the significance of coccyx health, common issues, and the pivotal role of physiotherapy in addressing coccyx-related discomfort. Our personalized approach, tailored treatment plans, and commitment to long-term well-being set us apart as leaders in coccyx physiotherapy.